HIMSS23 organizers led a content-rich, full-day educational event called the Interoperability and HIE Forum on Monday, April 17. Broken into six sessions, the forum included subject matter experts from a broad range of backgrounds, including government, healthcare delivery organizations, law, consortiums, and consulting firms. Session topics were:
- Health Data Utilities: Furthering Interoperability and Exchange in a Post-HITECH World
- Mergers, Partnerships, and the Evolving Healthcare Market
- Driving Interoperability in 2023: Cures, TEFCA, and Information Blocking
- Deep Dive into the Digital Front Door and Patient Access
- Advancing Health Equity Through Interoperability
- Optimizing Public/Private Collaboration to Scale What Works
As I suspect many in the audience did, I attended the forum seeking to become better informed professionally and personally. As a content creator for Rhapsody, I spend much of my time writing about the state of interoperability and how Rhapsody solutions help organizations overcome data exchange and data quality challenges.
And as a card-carrying member of the sandwich generation — tending to healthcare needs of my parents, myself, and my children — I was also personally curious about real-world, tangible advancements that might make managing my families’ health data easier.
I came away better informed on both fronts and share my takeaways in a series of blog posts, starting with this one on the Trusted Exchange Framework and Common Agreement, or TEFCA.
While there was a lot to celebrate in terms of TEFCA advancements, Qualified Health Information Networks (QHINs), and interoperability in general, it’s clear that there is still plenty of work to do before we’ll realize the benefits of TEFCA. TEFCA is aimed at amplifying the work HIEs are doing and further reducing the friction and costs associated with exchanging health data.
Need a TEFCA primer? Check out these resources.
- How State HIEs Are Advancing Interoperability | Rhapsody
- TEFCA: Everything Healthcare Organizations Need to Know | Rhapsody
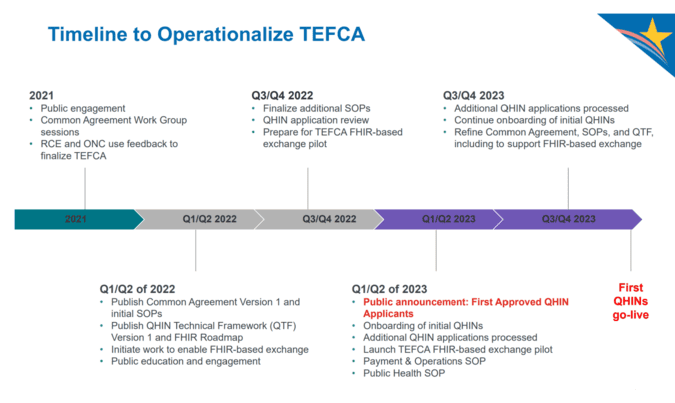
Lisa Bari, MBA, MPH, chief executive officer for Civitas, kicked off the forum with an opening keynote titled Health Data Utilities: Furthering Interoperability and Exchange in a Post-HITECH World. She walked the audience through milestones on a timeline of health IT and health information exchange (HIE) policies going back to the early 1990s with the rollout of electronic health records, all the way through to today and the announcement of first six organizations approved as QHINs.
She explained that while legislation and regulation over the last two decades points to nationwide centralization, consolidation, and an EHR-centric view of interoperability, community-governed health information exchanges (HIEs) fulfill critical roles that go beyond the goals of national interoperability networks and frameworks. HIEs have proven to work in connecting the private and public sectors, something we witnessed during the COVID-19 pandemic.
A HIMSS article from April 2020 noted, “Several national exchange efforts are contributing to the response, but as the U.S. deals with a pandemic that impacts each region differently, these regional HIE organizations play a vital role and can have a direct impact on a community’s preparedness and response to COVID-19.”
Bari said that data governance must happen at the community level with local stakeholders in line with state laws and local preferences.
For example, local HIEs enable surveillance over specific populations, including identifying diagnoses codes and other markers that can be used to alert public health agencies — which is different than the role national networks provide. HIEs also have the ability to produce analytics on information they’re ingesting, and then ultimately provide services, such as creating actionable reports, to local public health agencies to help follow specific disease progressions. This level of partnership was evident during COVID-19 and has since continued.
The role of state HIEs and public health agencies varies by state
Panelists from the next session, Mergers, Partnerships, and the Evolving Healthcare Market, underscored the importance of state and regional HIE participation. When an audience member asked Tim Pletcher, executive director of Michigan Health Information Network (MiHIN), whether any best practices from recent HIE consolidation in Pletcher’s region could be applied to other states with multiple HIEs, Pletcher responded that offering advice to states like California and Texas wouldn’t be appropriate because the populations are vastly different. Pletcher added that funding models vary quite a bit from state to state, as do the roles that individual counties play.
(Tim Pletcher also served as a panelist in this recent education session at Rhapsody. See what he and other leaders from HIEs shared in TEFCA Panelists Answer Looming Questions About the Trusted Exchange Framework and Common Agreement | Rhapsody)
Lean on interoperability and EHR vendors for HIE connection
Panelists in the Driving Interoperability in 2023: CURES, TEFCA, and Information Blocking session argued that providers shouldn’t have to know which path to follow to connect to QHIN. Rather, providers should know what their EHR and interoperability vendors are doing to ensure connectivity to TEFCA so it’s seamless and they don’t have to worry about duplication of data.
Advice for healthcare IT leaders: Participate in your local HIEs and lean on your vendors for guidance in TEFCA participation.
If you’re not sure where to begin with getting involved with state or regional exchanges, and eventually QHINs, look to your vendors, including Rhapsody, for help. HIEs rely on Rhapsody health solutions to gain a foundation for analytics and outreach programs, helping their partners to improve health equity. Check out these use cases to learn how.
