Interface engines provide flexibility to easily connect to the referring medical community
Imaging centers, hospitals, laboratories, and clinics are all faced with the demand of providing electronic patient data to maintain productive business relationships with the referring medical community.
Today, there are two approaches interfacing:
- Create point-to-point interfaces with application vendors
- Select an interface engine solution to connect all internal and external applications
Determining the most effective approach for healthcare integration has a long-term impact on an organization’s physician outreach programs, workflow efficiencies, operational costs, and overall client support.
Healthcare interfacing overview
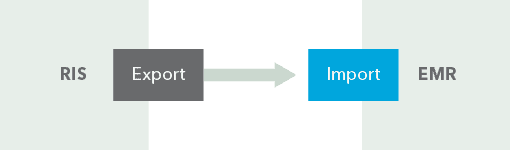
To facilitate communication between two healthcare applications, a modest interface includes:
- An export endpoint for the sending application
- An import endpoint for the receiving application
- A method of moving data between the two endpoints
- A method for handling the queuing messages
- A method for logging the flow of messages
HL7 is the most widely used data standard to facilitate the communication between two or more clinical applications. The prime benefit is that HL7 simplifies the implementation of interfaces and reduces the need for custom interfaces.
Below is a simple interface between an imaging center’s RIS and a hospital’s EMR.
Taking this example a step further, below is the same RIS and EMR systems but with the added capability in both applications to import and export data.
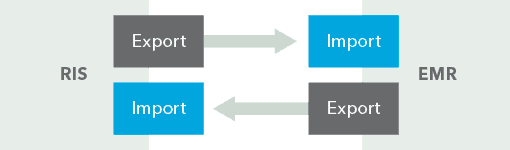
Logic tells us that each healthcare application must grant access to accept and send patient data and have rules of what it will accept and what it will send. This access to data is usually tightly controlled by each application vendor to ensure data integrity within their application.
Both of these examples are simple: one application exchanging data with another. However, the world of healthcare is not that simple. There are multiple applications and multiple providers in a healthcare organization and community. Each additional application and provider added to the network increases the interfacing complexity exponentially.
The complexity increases due to the hard-and-fast rules about how each application and provider will send and receive data. One export interface will not meet the requirements of every application. Similarly, one import interface will not meet the requirements of every application.
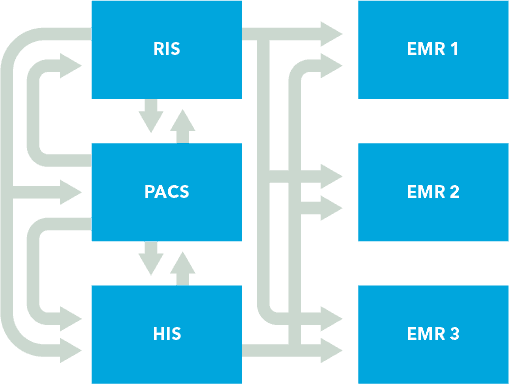
Point-to-point interfaces
A point-to-point interface is one in which the receiving vendor provides a specification on what data it can receive and in what format it needs to be in. The sending application then builds an interface to that specification for that application. It is a one-to-one relationship. For each application requiring an interface, there is a new request and point-to-point interface developed.
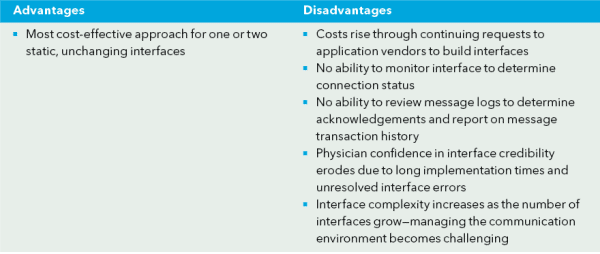
Illustrated below is a point-to-point interface environment.
Interface engine approach
An interface engine can transform or map the data according to the receiving application’s requirements so the data can be used by the receiving application.
Essentially, the import and export module from the sending application is built in a very comprehensive manner, capturing all potential data to be used in one interface. The application interface is built with a one-to-many concept in mind. These import/export modules then are connected to an interface engine so that the mapping, routing, and monitoring are managed by this system.
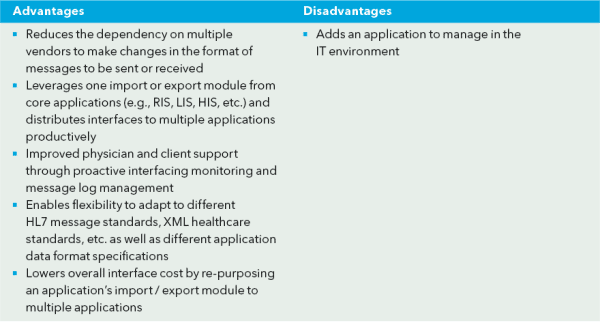
Illustrated below is an interface engine environment.

The ROI of interface engines
There are multiple ways an interface engine can help you leverage your organization’s investments.
One-payment to application vendors
The sending application (RIS, HIS, LIS) needs to be opened up to export and import data. These interfaces can be a one-time fee if they are defined broadly enough so that the interface engine has access to all possible data fields needed to map and transform the data to meet each application’s data specifications.
Independence and control
With an interface engine, new interfaces to applications and providers can be designed and implemented with the provider’s staff. Greater control over interfaces is gained by the providers, decreasing the reliance on application vendors for each and every interface.
Shortened cycle time
Implementing interfaces is completed on the your time schedule, not the vendors. Typically, with an interface engine, interface development and deployment cycle time is shortened from 6–12 months to 1–2 weeks. This gives imaging centers, laboratories, and hospitals a competitive advantage in reaching out to the referring community and delivering quickly to meet their EMR requirements.
Map and route messages for workflow and application requirements
Any data format that is sent or received can be transformed into the right format for any application. No modifications are required by each application vendor each time a new data specification is received. Business processing rules can be implemented to enhance and streamline workflows within the provider’s organization and externally.
Ease of monitoring and management
To keep customer support costs low, interface implementations should be easy to monitor to ensure consistent data flow. Track the uptime of critical interfaces, resolve issues proactively, and quickly fix issues through Corepoint Integration Engine.
Meet Meaningful Use requirements
Both Rhapsody and Corepoint Integration Engine allow providers to exchange data using common standards used in healthcare including Consolidated CDA and Direct Project, the two standards required in Meaningful Use.
Scalable
In a modern health IT environment, the number of needed interfaces will grow over time. An interface solution must be able to grow with the demands of your growing business.
