Healthcare searches for IT stability to manage and implement change
Abstract
Everyone involved in health IT knows that the industry is in a period of market consolidation and transformation. These changes are happening in all sectors, both within each sector and across them, as well.
- Hospitals are acquiring not only other hospitals but also physician practices
- Medical providers are opening accountable care practices that may function alongside still-operating, traditional fee-for-service models
- Electronic health record vendors are consolidating as the industry matures and successful vendors seek to increase their market share through acquisition
- Insurers continue to grow as a result to keep pace with large health systems
These moves pose many challenges for health IT.
How, for example, do CIOs know if longstanding vendors will be in existence 2, 3, or even 5 years down the road? What affect will vendor and provider consolidation have on patient care? How can we know where the industry is headed with so much in doubt with the government’s Meaningful Use program? How is it possible to become innovative during such tumultuous times?
Conclusion
Sustainable health IT systems depend on an interoperable health data layer that serves as the health data platform to exchange data between applications. While much attention has been placed on the EHR system, the integration layer serves as the catalyst for all health data activities and allows IT departments to break free from EHR “data siloes” and gain full control of their patients’ health data.
Once a health data framework is established through the integration layer, the IT team has access to a myriad of system performance information about the enormous amount of health data transmitted between systems and applications every day. Because integrating systems is no longer an obstacle, a hospital can become nimble and responsive, with their IT systems offering a distinct competitive advantage.
Topics included in this white paper:
- Meaningful Use uncertainty
- Hospital consolidation
- Health IT vendor consolidation
- Interoperability
- Strategic data frameworks
Healthcare shifts
The healthcare industry has experienced a great deal of change beginning in 2009 with the passing of HITECH, which was part of the America Recovery and Reinvestment Act. HITECH is an acronym for Health Information Technology for Economic and Clinical Health, and it introduced the industry to the government’s ambitious plan to encourage the “Meaningful Use” of electronic health records throughout the country.
Since that time the healthcare industry—perhaps especially health IT—has been in a period of constant change and, some would say, confusion. Hundreds of EHR vendors flooded the market in the beginning stages of Meaningful Use and hospitals and providers of all sizes lined up to purchase and implement the technology, encouraged by the government’s $36 billion reimbursement program.
However, the costs associated with implementing EHR systems escalated and Meaningful Use requirements expanded, putting pressure on many of the EHR vendors to add functionality that their software or their overwhelmed development staff were unable to support. This free-market response was predictable; unfortunately, it left many providers in a difficult situation with technology that is incompatible with the government’s demands or, worst case, out of business completely.
Yet another significant catalyst for change was introduced just one year later in 2010. The Patient Protection and Affordable Care Act, or “Obamacare,” injected the Accountable Care Organization model into the changes already taking place as a result of HITECH. According to the Centers for Medicare & Medicaid Services (CMS), an ACO “is an organization of health care providers that agrees to be accountable for the quality, cost, and overall care of Medicare beneficiaries who are enrolled in the traditional feefor-service program who are assigned to it.”
In short, ACOs are a value-based model of providing healthcare for patients rather than the traditional fee-for-service model that the industry has operated under since its inception. The value-based model of care is causing providers to change the way they bill for care—instead of being paid by the number of visits and tests they order (traditional fee-for-service model), their Medicare payments are now based on the value of care they deliver (value-based care).
Many argue that this change of direction is long overdue because it drives improvements to the delivery of care by mandating better care at a lower cost. However, it is yet another seismic change in the healthcare landscape that is shifting the foundation of the industry and causing significant uncertainty. It requires care coordination across many providers, which requires interoperability between EHR systems.
This uncertainty has brought a wave of market consolidation and transformation. These changes are happening in all sectors: Hospitals are acquiring other hospitals and also physician practices; medical providers are opening ACOs that operate alongside fee-for-service models; EHR vendors are consolidating as the industry matures and successful vendors seek to increase their market share through acquisition; and even insurers continue to grow to keep pace with the large health systems.
A large majority of these changes are placing an inordinate amount of pressure on healthcare technology departments that must support a growing and changing healthcare marketplace. This paper will examine some of the driving factors for uncertainty, including advice for healthcare IT departments to help them better manage the always changing technology landscape.
Meaningful Use uncertainty
The very program that initiated much of the change in healthcare in 2009 has run its course. In January 2016, the Centers for Medicare and Medicaid Services Acting Administrator Andy Slavitt made headlines when he said the Meaningful Use program is coming to an end in 2016. According to an article in Healthcare IT News, Slavitt said, “We have to get the hearts and minds of the physicians back. I think we’ve lost them.”
Mr. Slavitt is referencing physician groups who have voiced their displeasure over the government’s demands and have become disillusioned by their EHRs, their lack of interoperability, and the extreme complexity of both Meaningful Use and the Affordable Care Act.
In response, the Department of Health and Human Services in April 2016 issued proposed changes to the Medicare Access and Summary CHIP Reauthorization Act. The proposed rule designated the Merit-based Incentive Payment System (MIPS) as a replacement for Meaningful Use for physicians. With this proposed rule, the HHS wanted to address three central priorities moving forward:
- Improved interoperability along with the ability of physicians and patients to easily move and receive information
- Increased flexibility as compared to the Meaningful Use program
- User-friendly technology designed around physician workflows
Future emphasis of health IT will be on health data interoperability and information exchange, with importance placed on security of protected health information (PHI) and a requirement to give patients access to their health information through APIs (application programming interfaces).
Hospital consolidation
Recent trends have shown an increase in the number of hospital, health system, and clinic mergers.
While there are many notable system mergers, there are just as many non-merger hospital consolidations occurring that don’t make the headlines. There are myriad reasons for consolidation, but the most-cited reasons are costreduction purposes. Smaller clinics and hospitals can save millions on a new EHR system by partnering with a larger health system. Larger health systems can, in turn, create ACOs with a larger network of providers at their disposal and reap the financial rewards of the new value-based care model introduced in the Affordable Care Act.
According to the American Hospital Association, “Hospitals are reshaping the health care landscape by striving to become even more integrated, aligned, efficient and accessible to the community. Both public and private forces are fueling the drive toward greater integration and alignment. The need to become more efficient and obtain access to capital to meet these challenges is leading to more integration among hospitals, physicians and other providers.”
That quote offers many hints to health data interoperability. Healthcare consolidation can be a positive trigger to address IT management challenges, particularly the many silos of paper and EHRs across the organization. By rationalizing the storage and management of this health information, organizations believe costs can be recovered through the consolidation process.
By reducing vendors, a healthcare organization can, ideally, reduce expenses and repurpose staff to focus on more strategic initiatives. Consolidation also enables consistency across all aspects of information management and can help provide standard policies for data management.
Vendor consolidation
With healthcare enterprises consolidating and Meaningful Use coming to an end, vendor consolidation is inevitable. Many incumbent vendors will get squeezed out or acquired by larger vendors. Larger EHR vendors looking for more market share are buying competitors. Some more notable examples of this consolidation trend are Greenway purchasing Vitera Healthcare Solutions and Cerner acquiring Siemens.
This process began in 2016 prior to Meaningful Use Stage 2 attestation. EHR companies who launched to cash in on government incentive dollars ended support for their product, rather than sink additional development costs into the product. As a result, many physicians who adopted cheap products now have to replace software to remain competitive.
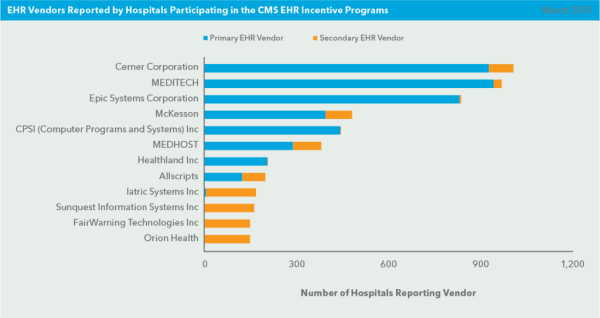
To illustrate, hospitals across the country have singled out a handful of EHR vendors to use as their primary EHR. According to the ONC, the following vendors dominate the market: Cerner, MEDITECH, Epic, McKesson, CPSI, MEDHOST, Healthland, Allscripts, and NextGen.
Today, we’re seeing the fallout of Meaningful Use and the beginning of the replacement market. This time, however, the providers searching for a new EHR system have the advantage—proven systems and vendors have well known and established track records. Providers are now able to choose the leading vendor for their particular niche, based on performance, responsive service and support, or a combination of all three factors. This approach to software selection is commonly referred to as the “best-of-breed” approach.
Healthcare’s best-of-breed vendors are recognized in the annual Best in KLAS: Software and Services report. Recognition as Best in KLAS is reserved for vendor solutions that lead various software and services market segments with the broadest operational and clinical impact on healthcare organizations. Utilizing KLAS rankings to health IT vendor selection has several advantages, including:
- Get the latest features and functions
- Leverage industry knowledge
- Reduce risk
- Increase system reliability
- Boost competitive advantage
The future of healthcare is exciting, and the changes will deliver new dimensions that will provide a more sustainable, high quality healthcare system. However, with uncertainty of the changes underway and the growing demand for broader health data exchange, there is no better time to have the right interoperability foundation in place.
It’s time for healthcare to adopt an interoperability-first approach
One of the largest obstacles in creating a value-based system is the current siloed and dispersed nature of integrated hospital IT applications and the myriad sources of patient data at each facility. Regardless of location, most EHRs or information systems were not designed to share data or to be interoperable with other systems.
It could be argued that the Meaningful Use program erred in not first requiring EHR systems to adhere to a strict health data standard to encourage the sharing of health data between systems. The government now appears to recognize the problems caused by the closed EHR databases that are prevalent across the country.
Dr. Karen DeSalvo, the National Coordinator for Health Information Technology and Director of the Office of the National Coordinator for Health Information Technology (ONC), wrote a blog post in 2015 on the ONC’s website titled, “Blocking of health information undermines health system interoperability and delivery reform.” In that article, Dr. DeSalvo highlights the importance of health data interoperability in a value-based system.
As the industry continues its shift toward valuebased care, the demands for health data have never been greater. However, with the uncertainty flooding the market thanks to facility and vendor consolidation, the rise of value-based care, and a shift away from the guidance of strict Meaningful Use requirements, hospital IT departments are left with expensive EHR systems and huge expectations from hospital leaders to leverage the data within those systems to lead to continued financial viability as the industry changes.
From population health management, to analytics programs, to patient-facing applications, health data is the cornerstone for value-based care. In order for that important foundation to support caregivers in patient care, that data must be made interoperable so that every application in use has the ability to send, receive, and access data.
Today’s healthcare IT departments need a central command unit—or an “eye in the sky”—to help guide the flow of data between applications and systems, and to ensure that each caregiver and colleague has the right patient data, with the right insights, at the right time.
Another needed shift may be from a bestof-breed mentality to creating a strategic data framework for IT operations. A Strategic Data Framework can facilitate and support the adaptability required to meet changing and growing demands.
Strategic data framework
Today’s high-quality, sustainable health IT systems depend on a strategic integration layer that serves as the health data platform to interoperate between applications. While much attention has been placed on the EHR system, the integration layer serves as the catalyst for all health data activities and allows IT departments to break free from EHR “data siloes” and gain full control of their patients’ health data.
With an independent strategic data framework, providers can act more interdependently with key IT initiatives, various vendors and partners, and patient delivery plans. The strategic data framework not only enables connected data flow but it empowers providers to meet any added industry changes with a solid foundation, flexibility, and freedom.
Once a health data framework is established through the integration layer, the IT team has access to a myriad of system performance information about the enormous amount of health data transmitted between systems and applications every day. Because integrating systems is no longer an obstacle, a hospital can become nimble and responsive, with their IT systems offering a distinct competitive advantage. Integration is no longer the shackles that threaten a CIO’s livelihood.
Advantages of establishing a strategic data framework to create stability in IT operations:
- Updates can be rolled out without affecting other systems
- Quickly respond to market changes
- Easily parse, integrate, and exchange data between applications, systems, and locations
- Quickly implement the best solutions at the clinical application layer, allowing other departments to make technology choices that compliment and improve workflows.
The secure, appropriate, and efficient sharing of electronic health information is the foundation of an interoperable learning health system—one that uses information and technology to deliver better care, spend health dollars more wisely, and advance the health of everyone.
As healthcare is set to adopt modern exchange standards in HL7 FHIR, the future “API economy” means that CIOs can reap the benefits of choosing the right technology for the job.
Foundation of interoperability
Infrastructure. It sounds like a commodity and is often treated as such in IT departments. Yet, without infrastructure, innovation and advancement is impossible.
Interoperability technology serves as the infrastructure for forward-thinking healthcare organizations. Calling it infrastructure, while not very exciting, is a solid description for how value-based healthcare organizations use an interoperable data foundation from which to manage all patient data activities. The biggest difference between today and 2009, when Meaningful Use was first introduced, is that care organizations are moving beyond the “good enough” approach to interfacing and are looking at integration engines as an innovative way to find new approaches that solve business and operational issues.
Moving beyond yesterday’s mindset of simple interface connectivity and into an innovative strategic data framework is key for value-based care. This change can only be achieved when key elements are present: an integration solution, a connected community solution, a workflow logic solution, and decision support capabilities. The cooperative interaction within this type of IT infrastructure enables strategic support by:
- Facilitating data collection and analysis for any connected application or vendor
- Creating real accountability within and outside of your hospital through analysis of data trends
- Decreasing operational costs by using centralized, interoperable data to support defined strategic goals
- Providing the ability to easily and quickly scale to meet new data demands and integration requirements
- Improving turnaround time for patients, departments and all community of care relationships
With the check-box approach of meeting Meaningful Use requirements finally in the rear view, innovative organizations are looking to create healthcare interoperability in a productive manner that operates as a strategic framework, rather than simply the “pipes” of the last generation’s approach to interfacing. This new approach is the key to achieving any strategic plan involving the use of health data, and provides unmatched flexibility and freedom for innovation.
Flexibility
IT Infrastructure can be thought of as having either a low or high ability to align your IT capabilities with strategic and operational goals. Some solutions only create incremental performance improvements. Leading interoperability solutions move beyond minor improvements and into providing a means to create a strategic data framework.
Leading hospitals and clinics benefit from this framework with the simple creation of robust interfaces in hours rather than days, connectivity that extends outside the four walls without limitations, and data that can be used as insights rather than as static information that is too-often ignored or unseen by caregivers.
While yesterday’s solutions enabled basic interfaces, a thoroughly developed data framework provides advantages:
- Leverage to extend quickly outside the four walls of your organization and establish electronic communication with your referring community
- Support for an unlimited number of integrated applications, enabling you to successfully meet growing demands for connected care
- Low learning curves and scalability costs, and elimination of special programming skills for IT staff
- Connecting to remote locations, leveraging newer technologies and communication vehicles
A strategic framework should support easy scalability, wide compatibility to a variety of data standards, and minimal increases in costs as your organization’s data demands increase. Adopting this level of infrastructure allows organizations to increase overall capacity and connect to remote facilities, which balances out cost and resource requirements.
A strategic data framework allows all patient data to come together for streamlined efficiencies in your organization.
Freedom to innovate
Using the right IT infrastructure allows leading organizations to move from average to exceptional, simply by harnessing patient data as a foundation for success. This gives IT leaders the freedom to help caregivers provide smarter healthcare—the driving force behind the current shift to value-based care.
The freedom to innovate and adapt to changing needs using patient data will receive significant attention in the coming years. Providing value-based care through accountable care models requires the ability to do more with patient data, not limitations that constrain progress.
The freedom provided by implementing a strategic data framework is fueling value-based organizations, allowing them to achieve what was unimaginable just 10 years ago, including the ability to:
- Develop ways to measure clinical quality in each inpatient and outpatient department
- Provide data directly to patients, making them a key player in the care process
- Monitor physician performance and trends
- Demonstrate widespread improvement with quantitative data
- Create better clinical documentation for patient records
- Exchange data with the greater healthcare community
- Develop more business partnerships with physicians
- Establish connected clinics in new communities
- Add in custom-built apps designed for clinicians or patients
An innovative, interoperable infrastructure is the ground floor of innovation in healthcare. Complaints about data hoarding and EHR data siloes become irrelevant, allowing leading organizations to broaden strategic plans with connected data and the insights it provides.
Conclusion
Leading organizations now recognize the value in establishing a strategic data framework that provides an interoperable, flexible data foundation that can be used to meet all future data demands. This approach ensures interoperability between systems and provides actionable insights to data and access to siloed EHR databases.
A fresh look at infrastructure translates to improved capabilities and a more connected healthcare community, allowing leading organizations to connect data to caregivers in the most efficient and effective manner possible.
