What is your data integrity model?
Demand for healthcare interfaces is rising, and there is a rapid pace in which healthcare entities are working to connect various internal applications and external resources. In a hospital environment, connecting the Electronic Health Record (EHR) to the Radiology Information System (RIS) to the Laboratory Information System (LIS) to the Hospital Information System (HIS) is one example of typical hospital workflow.
Today, healthcare interoperability initiatives are shifting more and more to external requirements. This shift is largely due to the passage of HITECH and the implementation of Meaningful Use. More practically, many healthcare organizations were already connecting externally. An external laboratory may be delivering lab test results electronically to a hospital system or a physician’s Electronic Medical Record (EMR) application is delivering patient information to a hospital system. In either scenario, there may be data integrity concerns as the data is no longer controlled entirely by the initiating hospital or other organization.
HL7 is the standard method to define the clinical messages sent between the applications and the institutions. Beyond clinical messages, other healthcare standards come into play including Continuity of Care Document or Record (CCD or CCR), X12, NCPDP, and the list goes on. With the growing number of standards, interfaces, and connections to different healthcare entities, instilling solid data integrity practices throughout the process is critical.
Why is this critical? Without the right data integrity model, the confidence in the deployed interfaces will be low and the support costs will be high. Clinical data not received properly, or received in an untimely manner, will quickly erode the healthcare professionals’ outlook on future healthcare interfaces and raise concerns regarding the quality of the data being exchanged.
Clinical data integrity model
There are several aspects to ensuring a robust data integrity model, and one way to look at it is based on two dimensions—Interface Testing and Interface Monitoring. Interface Testing is the practice of ensuring that the interfaces being developed are of the highest quality prior to deployment. Interface Monitoring is the practice of ensuring that the interfaces continue to operate with a high degree of integrity after deployment. Together, these two practices ensure the highest integrity for the connected healthcare environment.
The image below explains the Clinical Data Integrity Model.
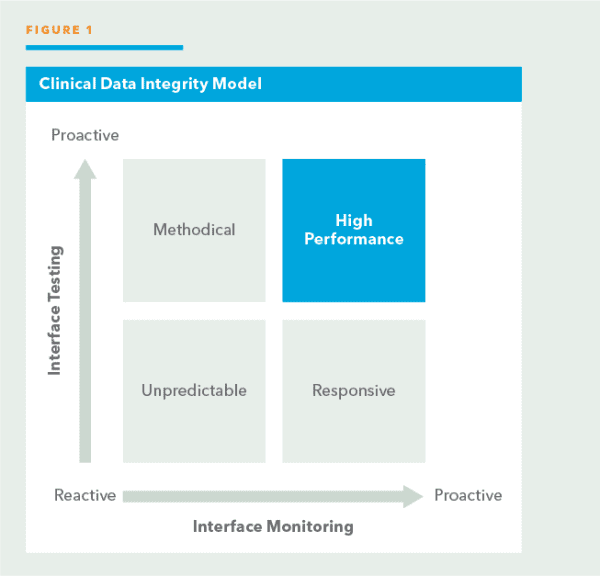
Depending on the quadrant that a healthcare institution may be in, different characteristics can be defined to the data integrity state. Ideally, the institution will want to be in the top right quadrant— High Performance—which means an equally proactive discipline to both Interface Testing and Interface Monitoring.
Data integrity model characteristics
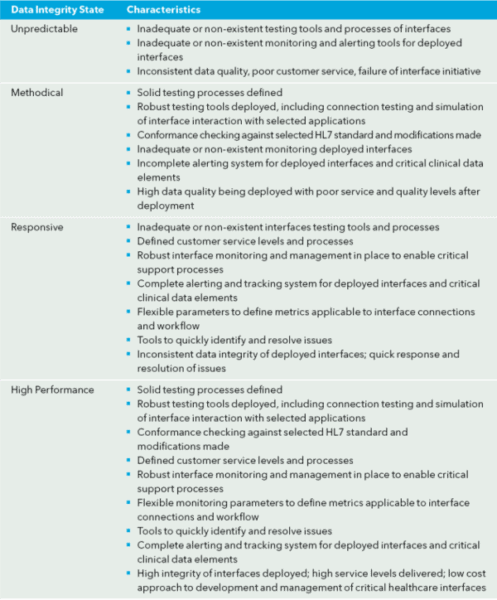
The characteristics for each quadrant are outlined in the following manner:
Summary
Why does being in the High Performance quadrant matter? The following five points summarize the importance of having implemented the right data integrity model:
- Clinical data sent to another healthcare application or entity is received as intended.
- Clinical data received from another healthcare application or entity is accepted as it is defined.
- Healthcare interfaces are fully tested and documented before being deployed.
- Interfaces are developed efficiently within requirements—the selected HL7 standard version and modifications included, as well as other healthcare standards such as CCD, CCR, CDA, X12, NCPDP, and the list goes on.
- Messages are exchanged in a timely manner. Bottlenecks or potential problem areas are identified quickly and proactively repaired. Healthcare departments and external entities (e.g., clinics, imaging centers and laboratories) receive high performing customer service which boosts their confidence in the integrity of the data used.
There are many initiatives unfolding which are driving greater demand for healthcare integration from Meaningful Use to EMR connectivity to Health Information Exchange (HIE) participation. Being in the High Performance quadrant is no longer optional; it is a necessity in order to deliver on today’s demands.
